Abstract
Our understanding of how individual mutations, whether present in all or just a fraction of the leukemia cells, affect cellular responses to therapy is limited. Leukemia mouse models provide a unique possibility to explore how therapy affects the evolution of genetically distinct clones and identify mechanisms of resistance allowing transfer to human disease. Herein, we studied how different therapies influenced survival, clonal evolution, and resistance patterns in mouse KMT2A-MLLT3 leukemia with subclonal FLT3 N676K.
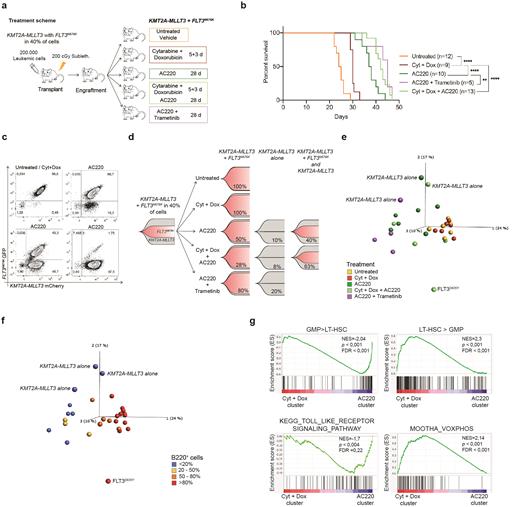
Bone marrow (BM) from a leukemia expressing KMT2A-MLLT3-mCherry in all cells and a FLT3 N676K-GFP in 40% of cells, were re-transplanted to sublethally irradiated recipients (Hyrenius-Wittsten el al, Nat Commun, 2018). Upon engraftment, treatment was started with either chemotherapy (cytarabine for 5 days + doxorubicin for 3 days), the FLT3 inhibitor AC220, chemotherapy followed by AC220, or AC220+Trametinib, a MEK inhibitor. Targeted treatment was given for 28 days; controls received vehicle (Fig. 1a). Survival was estimated by Kaplan-Meier and the developing leukemias were analyzed by flow-cytometry, RNA-sequencing and targeted gene re-sequencing.
Each treatment prolonged survival with a median latency of 30 days for chemotherapy , 37.5 days for AC220, 42 days for chemotheraphy+AC220, and 45 days for AC220+Trametenib, versus 25.5 days for the control (Fig. 1b). Most leukemia cells expressed GFP/mCherry and mice displayed splenomegaly and leukocytosis.
Next, we investigate how treatment impacted evolution of the KMT2A-MLLT3+FLT3 N676K cells and while they constituted all cells in control and chemotherapy-treated mice, the other treatments impacted their evolution. Three distinct patterns were discerned with either >80% of KMT2A-MLLT3+FLT3 N676K cells, >80% of cells expressing KMT2A-MLLT3 alone, or dual similar sized clones of cells expressing KMT2A-MLLT3 alone or KMT2A-MLLT3+FLT3 N676K(Fig. 1c). Eradication of the FLT3-leukemia cells was rare, but most common in mice receiving AC220+Trametinib and the frequency of dual clones increased when mice received chemotherapy followed by AC220, in line with treatment selectively affecting evolution of genetically distinct cells (Fig. 1d).
To find clues to treatment resistance, RNA-sequencing (N=44) revealed segregation into three major clusters: 1) leukemias expressing KMT2A-MLLT3 alone, 2) control and chemotherapy-treated leukemias and 3) AC220 treated leukemias. Notably, a set of AC220-treated mice clustered close to the control and chemotherapy-treated mice (Fig. 1e). Flow-cytometry data showed that similar to the control and chemotherapy-treated leukemias, the myeloid BM cells of those AC220 samples, aberrantly expressed B220 (Fig. 1f). Gene set enrichment analysis revealed enrichment of gene sets correlating with stem cells and oxidative phosphorylation in those AC220-treated leukemias, suggesting a switch in cellular phenotype and metabolic state upon treatment. By contrast, the other AC220 leukemias (cluster 3), instead showed enrichment of gene sets correlating with granulocyte/macrophage progenitors and immune regulatory pathways, indicating selective dependence of distinct cellular pathways upon resistance (Fig. 1g). Finally, acquisition of AC220 resistance mutations was rare with a FLT3 D835Y and a Ptpn11 G503V detected in two leukemias only.
Taken together, these results show that the specific treatment given not only affected survival of the FLT3 N676K mutated KMT2A-MLLT3 leukemia, but also impacted how the genetically distinct cells evolved. The general lack of acquired mutations upon targeted treatment suggests that target-independent mechanisms that result in alternate activation of survival/proliferation explains acquired resistance in a majority of mice and provides novel insights into treatment resistance.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal